An Essential Guide to Help for Veteran Suicide
- Gary Otte
- Aug 1
- 11 min read
Why Understanding Veteran Suicide is Critical for Our Communities

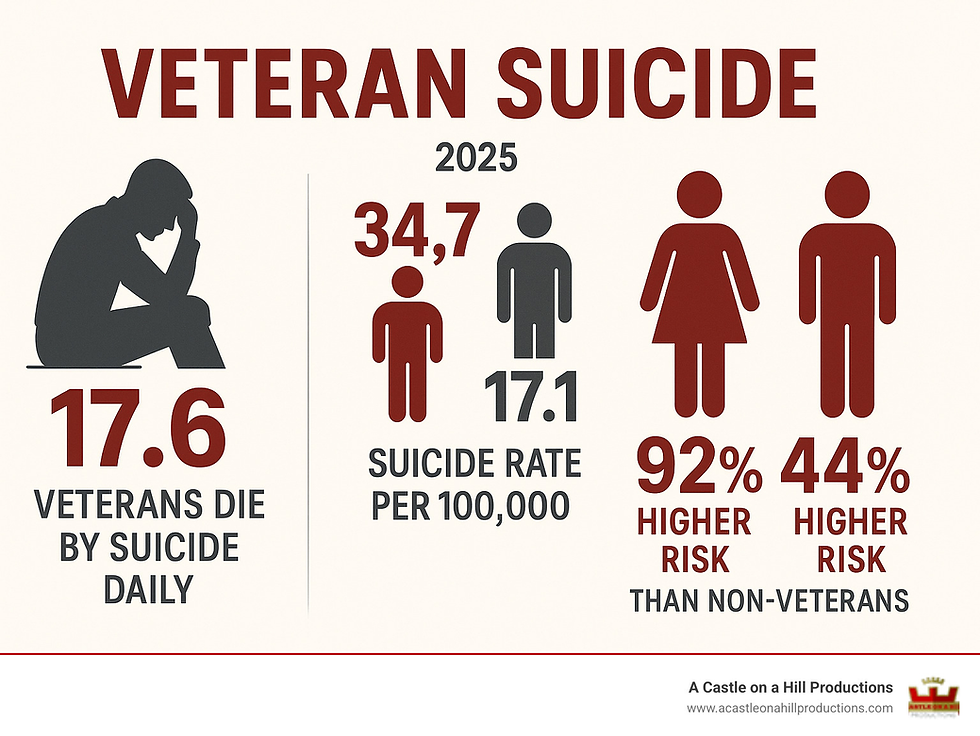
Veteran suicide represents one of America's most pressing public health crises, claiming the lives of approximately 17.6 veterans every day. This devastating reality affects not just the veterans themselves, but their families, communities, and our nation as a whole.
Key Facts About Veteran Suicide:
6,407 veterans died by suicide in 2022
Veteran suicide rate is 34.7 per 100,000 - nearly double the rate of non-veterans (17.1 per 100,000)
Female veterans are 92% more likely to die by suicide than non-veteran women
Veterans aged 18-34 have the highest suicide rate at 47.6 per 100,000
74% of veteran suicides involve firearms
Only 40% of veterans who die by suicide had recent contact with VA healthcare
The statistics paint a sobering picture, but they also tell us something important: veteran suicide is preventable. Behind every number is a person who served our country, and understanding the scope of this crisis is the first step toward meaningful action.
Veterans face unique challenges when transitioning to civilian life. The loss of a structured environment, purpose, and camaraderie, combined with potential trauma and injuries, creates a complex web of risk that requires our understanding.
This guide provides essential information about veteran suicide - from recognizing warning signs to understanding available resources and prevention strategies. Whether you're a veteran, a family member, a healthcare provider, or simply someone who cares about those who served, this information can help save lives.
I'm Gary Otte. Through my work in video production, I've told stories that matter, including those highlighting veteran experiences and mental health awareness. Understanding veteran suicide is crucial for supporting those who served.
Understanding the Scale of the Veteran Suicide Crisis
Veteran suicide is a public health crisis demanding our attention. The alarming trends and disproportionate impact on veterans highlight a critical need for awareness and intervention. By understanding the numbers and the demographics most affected, we can foster a more supportive environment for those who have served.
Alarming Statistics: A Look at the Numbers
The latest data paints a stark picture. In 2022, 6,407 veterans died by suicide in the U.S. The suicide rate for veterans is 34.7 per 100,000—nearly double the rate for non-veterans (17.1 per 100,000). Since 2005, the suicide rate among veterans has risen faster than for non-veteran adults.
The Department of Veterans Affairs (VA) conducts the largest national analysis of veteran suicide rates each year. Their annual reports, like the 2023 National Veteran Suicide Prevention Annual Report, are foundational to our understanding of this crisis. While the overall numbers are sobering, they also provide crucial insights into where our efforts need to be focused.
Who is Most at Risk? Key Demographics
Veteran suicide doesn't affect all veterans equally. Certain demographics face significantly higher risks, and understanding these differences is key to developing effective prevention strategies.

A striking disparity is found in age. While older veterans (age 55+) accounted for 60 percent of all veteran suicides in 2022, the rate tells a different story. Younger veterans, aged 18–34, had the highest suicide rate: 47.6 per 100,000 in 2022, following a 95.3% increase between 2001 and 2020. This points to a severe crisis during their early post-service years. Older veterans, especially from the Vietnam era, also carry unique burdens, including the lingering effects of war and feeling forgotten, which can compound mental health challenges.
Gender also plays a significant role. The suicide rate for male veterans was 44 percent higher than for nonveteran men in 2022. The disparity is even more pronounced for female veterans, whose suicide rate was an alarming 92 percent higher than for nonveteran women in 2022, making their rate 2.5 times higher than non-Veteran adult women. This highlights the urgent need for prevention efforts designed for women.
Other factors that significantly increase risk include:
Recent separation from service: The transition from military to civilian life can be incredibly challenging. The suicide rate for veterans in the 12 months following military separation was 46.2 per 100,000 in 2021. This period often involves a loss of identity, camaraderie, and a structured environment, leading to feelings of disorientation and isolation.
Other than honorable discharges: Veterans with "other than honorable" discharges face unique barriers to accessing VA services and community support. Research shows their suicide rates are twice as high as those with honorable discharges.
Race and Ethnicity: Some racial and ethnic groups have seen disproportionate increases in suicide rates. For instance, Asian, Native Hawaiian, and Pacific Islander veterans had a 259% increase in their suicide rate since 2002, and American Indian and Alaska Native veterans saw a 145% increase. These trends highlight the need for culturally competent outreach.
Understanding these demographic nuances is crucial for tailoring prevention efforts and directing resources to the most vulnerable. Whether in Kansas City, Billings MT, or Colorado Springs, every veteran deserves informed and compassionate support.
Key Risk Factors and Warning Signs for Veteran Suicide
Veteran suicide is rarely caused by a single issue, but rather a combination of personal, social, and environmental factors. Understanding these risk factors and the specific warning signs is vital. It empowers us to offer support when it matters most, potentially saving a life.

Common Contributing Factors to veteran suicide
Certain challenges stand out when we look at why veteran suicide occurs. These factors can weigh heavily on a veteran, and understanding them helps us approach the issue with more empathy.
Mental Health Conditions like Posttraumatic Stress Disorder (PTSD), depression, and anxiety are strongly linked to veteran suicide. Among veterans receiving VA care, about 40 percent had a mental health or substance use disorder in the year leading up to their death. The connection is powerful, but these conditions are treatable. Reaching out for help is a sign of courage.
To learn more, the VA has information on The Relationship Between PTSD and Suicide.
Substance Misuse is another factor. Veterans struggling with drugs or alcohol are more than twice as likely to die by suicide compared to other veterans. Often, substance use disorders co-occur with mental health conditions, creating a cycle that increases risk.
Traumatic Brain Injury (TBI) from combat or other military incidents is a recognized risk factor. The risk of suicide or suicidal thoughts increases with the severity or number of TBIs.
Military Sexual Trauma (MST), including sexual assault or harassment during service, significantly increases suicide risk. For veterans who experienced MST, the suicide rate was 25.0 per 100,000 in 2022. MST affects all genders, and for male veterans, the rate was even higher at 75.5 per 100,000.
Homelessness and Financial Strain are huge stressors. Veterans with low income have consistently shown the highest suicide rates among VA patients. Veterans who have been homeless were found to be almost 8 times more likely to have attempted suicide.
Other contributing issues include chronic pain, sleep problems, increased health problems, relationship problems, and feelings of hopelessness. The reasons behind veteran suicide are complex, involving biological and psychological factors.
Recognizing the Warning Signs
Knowing the warning signs is incredibly important. If you see these indicators in a veteran, it's a critical moment to reach out. Your observation could make all the difference.
Here are some key warning signs to look for:
Talking about wanting to die or to kill themselves: This is the most direct and serious sign. Always take it seriously.
Looking for a way to kill themselves: This could involve searching online for methods, or trying to get a firearm or other means.
Talking about feeling hopeless or having no reason to live: They might express a deep sense of despair or that life just isn't worth living anymore.
Talking about feeling trapped or being in unbearable pain: They might describe a situation where they see no escape from their suffering.
Talking about being a burden to others: They might believe their loved ones would be better off without them.
Increasing the use of alcohol or drugs: Using substances more often to try and cope with overwhelming emotions.
Acting anxious or agitated; behaving recklessly: Showing extreme restlessness, or engaging in impulsive, dangerous activities.
Sleeping too little or too much: Noticeable and significant changes in their usual sleep patterns.
Withdrawing or isolating themselves: Pulling away from friends, family, and activities they once enjoyed.
Showing rage or talking about seeking revenge: Exhibiting intense anger or expressing thoughts of vengeance.
Displaying extreme mood swings: Rapid and intense shifts in their emotional state.
Giving away prized possessions: This can be a sign they are preparing for their absence.
Saying goodbye to people: Making unusual or final goodbyes, especially if they seem out of character.
For a more complete list, we recommend checking out the American Foundation for Suicide Prevention Warning Signs. If you spot these signs, reaching out quickly can save a life.
Pathways to Prevention and Support
Veteran suicide is preventable through a proactive, multi-faceted approach involving institutions and communities. We are committed to highlighting available resources and fostering a culture where seeking help is the norm.
VA and Government-Led Initiatives
The Department of Veterans Affairs (VA) is at the forefront of preventing veteran suicide, implementing a wide range of programs.
Veterans Crisis Line (988 then Press 1): This is a 24/7, confidential resource for veterans in crisis or those concerned about a veteran, accessible by phone, text (838255), or online chat. The suicide rate in the first month following documented Veterans Crisis Line contact in 2021 was 22.5% lower than in 2019. This line is available to all veterans, regardless of their enrollment in VA healthcare.
VA Mental Health Care: The VA provides comprehensive mental health services, using universal suicide screening programs like Risk ID to identify veterans at risk. The VA also employs predictive algorithms through programs like REACH VET for proactive outreach. However, 90% of veterans who died by suicide were not classified as high risk by REACH VET, highlighting the need for broader approaches.
Transition Assistance Program (TAP): TAP presents an opportunity to educate separating personnel about mental health resources and safe firearm ownership practices.
"Caring Contacts" Program: This VA initiative sends brief messages of support to at-risk veterans. While it has been shown to increase healthcare utilization, it has not yet demonstrated a significant effect on future suicide attempts.
Challenges Reaching Non-VA Users: A significant limitation is reaching veterans not engaged with the VA system. In 2022, 60% of veterans who died by suicide had no VHA encounter in the year of death or the prior year. This group presents a critical challenge.
Overall Effectiveness: The age- and sex-adjusted suicide rate among Veterans with recent VHA use decreased by 2.4% between 2017 and 2018, while it increased by 2.5% among Veterans who did not use VHA care, suggesting engagement with VA care can be a protective factor.
You can find more detailed information on VA Suicide Prevention resources.
The Critical Role of Firearm Safety in veteran suicide
A highly impactful area for prevention is firearm safety. Firearms were involved in 74 percent of veteran suicides in 2022. Easy access to lethal means during a crisis can be the difference between a temporary struggle and a permanent tragedy.
Lethal Means Safety: This concept focuses on creating time and distance between a person in crisis and highly lethal methods, which for veterans, overwhelmingly means firearms. Responsible gun ownership includes safety measures to prevent harm.
Safe Storage Options: Promoting secure storage is paramount. This includes gun locks, gun safes, and off-site storage (temporarily storing firearms with a trusted person or facility during a crisis). Alarmingly, 53% of veteran gun owners do not store all of their guns securely.
Extreme Risk Laws (Red Flag Laws): These laws allow for the temporary removal of firearms from individuals deemed a danger to themselves or others by a court. Studies have shown their effectiveness, with one finding a 14% reduction in Connecticut’s firearm suicide rate and another associating Indiana's law with a 7.5% decrease.
Clinician Conversations: Healthcare professionals have a vital role in discussing firearm safety. A majority of U.S. gun owners, including veterans, agree that it is appropriate for clinicians to talk about firearm safety with patients.
For more information and data on this critical topic, we refer to Everytown Support Fund research on firearm suicide.
Community and Non-Governmental Support Systems
Community-based and non-governmental efforts are also vital in preventing veteran suicide. These organizations fill gaps, provide local support, and reach veterans who may not use the VA system.
Peer Support Networks: Programs like "Together With Veterans" (TWV) empower veterans to lead suicide prevention efforts in their own communities.
Vet Centers: These centers provide free, confidential counseling and outreach to veterans and their families in a community-based, non-medical setting. Readjustment Counseling (Vet Centers) offers support for a wide range of issues.
Non-Profit Organizations: The Staff Sergeant Parker Gordon Fox Suicide Prevention Grant Program allocated $174 million to 91 organizations to provide community-based suicide prevention services.
Governor's and Mayor's Challenges: These initiatives foster collaboration between state/local leaders, VA, and community partners to implement suicide prevention plans custom to their veteran populations, such as in Dallas or Colorado Springs.
Faith-Based Groups: Many faith communities provide social support, a sense of belonging, and spiritual guidance, which can be protective factors.
These community efforts are essential because they provide diverse entry points for help, reduce stigma, and build a stronger safety net.
Frequently Asked Questions about Veteran Suicide
It's natural to have questions about a topic as sensitive as veteran suicide. Here, we address some of the most pressing ones to empower you to make a difference.
What is the single most important thing I can do if I think a veteran is suicidal?
The single most important thing you can do is to ask directly if they are thinking about suicide. While it may feel uncomfortable, asking directly shows you care and can open the door for them to talk about their pain.
If they share their thoughts, listen without judgment. Stay with them; do not leave them alone. If possible and safe, discreetly remove any lethal means from their immediate environment, such as firearms or medications. Finally, connect them to help. The Veterans Crisis Line (988 then Press 1) is a 24/7, confidential lifeline. You can call for them or help them make the call. These immediate steps can be life-saving.
Are veterans who don't use the VA eligible for any suicide prevention help?
Yes. Many veterans are not enrolled in VA healthcare, but they are still eligible for suicide prevention help.
The Veterans Crisis Line (988 then Press 1) is for all veterans, regardless of their VA enrollment status. Vet Centers also provide free, confidential counseling to veterans and their families, operating separately from VA hospitals. You don't need to be enrolled in VA healthcare to access their services.
Additionally, countless community-based non-profit organizations across the country specialize in veteran support. The COMPACT Act has also expanded access to emergency mental healthcare for veterans, ensuring they can receive immediate care at VA or community facilities, even if they're not regular VA users.
How can I support a veteran who refuses to talk about their struggles?
It can be worrying when a veteran you care about is struggling but refuses to open up. It's important not to give up hope.
First, be patient and persistent. Building trust takes time. Express your concern gently, using "I" statements, such as, "I've noticed you seem withdrawn lately, and I'm concerned about how you're doing." This focuses on your feelings rather than making them feel accused.
Offering practical help can break the ice, such as helping with errands or bringing over a meal. Encourage connection, without pressure by inviting them to low-key social activities. Just knowing you're there can be comforting.
You can also share resources discreetly, leaving information about the Veterans Crisis Line or a local Vet Center where they might find it. Most importantly, reassure them you are there for them and that they are not a burden. Your genuine presence and concern can make all the difference in preventing veteran suicide.
Conclusion: A Call to Action for Hope and Healing
The issue of veteran suicide is complex, but it is not impossible. Suicide is preventable, and our collective responsibility is to ensure every veteran feels supported and has access to the resources they need.
We must work to reduce the stigma around mental health, especially in the veteran community where a culture of self-reliance can be a barrier to seeking help. Fostering connection is a powerful protective factor. Every act of support, from official programs to a simple personal outreach, contributes to a stronger safety net.
At A Castle on a Hill Productions, we believe in the power of compelling storytelling to shed light on critical issues and inspire action. We've seen how narratives can bridge understanding, reduce isolation, and encourage hope. Just as we strive to create impactful films, documentaries, and commercials, we are equally committed to raising awareness about vital causes like veteran suicide.
Let us remember that every veteran deserves a life of peace and well-being. By staying informed, being vigilant, and extending a hand of support, we can work towards a future where fewer veterans are lost to suicide. There is hope, there is help, and together, we can make a difference.
If you're interested in how powerful storytelling can transform perception and ignite change, we invite you to Learn how compelling video storytelling can raise awareness for important causes.




Comments