Navigating the Darkness: A Comprehensive Guide to Understanding Suicide
- Gary Otte
- Aug 1
- 10 min read
Understanding the Reality of Suicide

Suicide, the act of intentionally causing one's own death, is a pressing public health challenge. In 2021, over 48,000 people died by suicide in the United States—one death every 11 minutes. In Canada, about 4,500 people die by suicide annually, or 12 deaths per day.
Key Facts About Suicide:
Definition: Intentionally causing one's own death
Suicide attempt: Non-fatal self-harm with intent to die
Suicidal ideation: Thoughts of ending one's life
Impact: For every death by suicide, many loved ones are significantly affected
Prevention: Suicide is preventable with proper support and intervention
Behind each statistic is a person who was struggling with unbearable emotional pain. Research shows suicidal individuals are often "blinded by feelings of self-loathing, hopelessness, and isolation" and "can't see any way of finding relief except through death."
Suicide affects families, friends, and entire communities. It's a leading cause of death for people aged 10-54 and carries an economic burden of over $500 billion annually in the U.S. But what matters most is that suicide is preventable. Most people with suicidal thoughts don't want to die—they want their pain to end. With proper support and treatment, lives can be saved.
This guide will help you understand suicide, recognize warning signs, know how to help, and learn about available resources. This information can make a difference.
Understanding the Scope and Language of Suicide
When we talk about suicide, the words we choose matter. Using respectful language creates space for healing and understanding. Let's clarify the key terms.
Suicide is the intentional act of ending one's own life.
Suicidal ideation refers to thoughts about ending one's life, ranging from fleeting wishes to detailed plans.
A suicide attempt is a non-fatal effort to end one's life. Every attempt is a cry for help that requires immediate compassion and professional support.
Non-suicidal self-injury (NSSI), such as cutting or burning, is intentional self-harm without the intent to die. It is a serious warning sign of overwhelming emotional distress.
We say someone "died by suicide" rather than "committed suicide." The word "committed" implies a crime, adding shame to grieving families. This respectful language is crucial. Globally, suicide is a major cause of death, and no community is immune.
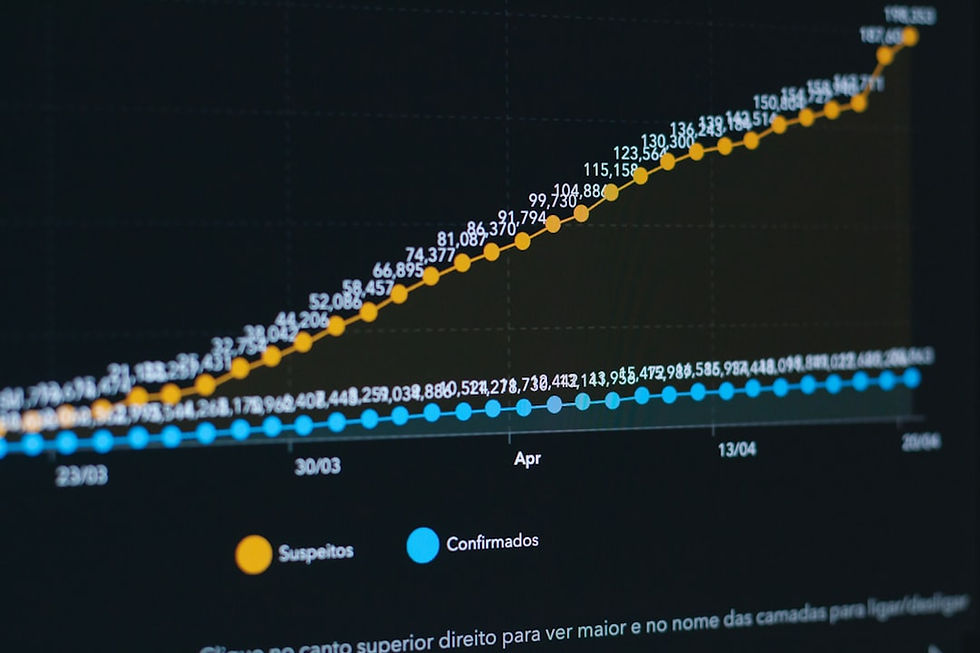
Suicide Statistics in the U.S. and Canada
The numbers are urgent. In 2021, the United States lost 48,183 people to suicide—one person every 11 minutes. In Canada, about 12 people die by suicide daily, totaling around 4,500 deaths each year. For every death, there are many more attempts.
For young people, suicide is a leading cause of death. It is the second leading cause for ages 10-14 and 25-34, and the third for ages 15-24. The COVID-19 pandemic worsened this trend, with the percentage of Canadian adults reporting suicidal thoughts increasing from 2.7% in 2019 to 4.2% in spring 2021.
Certain patterns emerge in the data:
Gender: Men die by suicide three to four times more often than women, though women and girls attempt suicide more frequently.
High-Risk Communities: Indigenous communities (First Nations, Métis, and Inuit), LGBTQ+ individuals (especially transgender youth), and autistic people face significantly higher risks. Veterans, rural residents, and workers in industries like construction also show higher rates.
For the most current data, the CDC suicide prevention webpage offers comprehensive statistics and guidance.
The Ripple Effect
When someone dies by suicide, the impact spreads widely. Each death significantly affects many loved ones, leaving them with complex grief, often called suicide bereavement. This grief can include guilt, anger, and a profound sense of abandonment.
The loss is felt by entire communities, including schools and workplaces. The economic toll is also staggering, exceeding $500 billion in the U.S. in 2020 due to medical costs and lost productivity. Grief and bereavement support, such as that offered by organizations like Bereaved Families of Ontario, is crucial for helping people steer this difficult journey. Preventing a single suicide protects an entire network of people from immeasurable pain.
Recognizing the Signs: Risk Factors and Warning Signs
Understanding what to look for can save lives. Think of risk factors as underlying conditions that increase vulnerability over time (like mental health disorders or trauma), while warning signs are immediate signals of acute risk that require urgent action.
Conversely, protective factors act as a safety net. Strong social connections, access to mental healthcare, good coping skills, and a sense of purpose all help protect against suicide.
Common Warning Signs of Suicide
Most people who attempt suicide show warning signs. These often appear in what they say, how they act, and their overall mood.
Talk: Listen for expressions of hopelessness, feeling trapped, or being a burden to others. They might talk about wanting to die or mention suicide directly.
Behavior: Watch for increased substance use, social withdrawal, reckless actions, giving away possessions, or saying goodbye. A sudden, unexpected improvement in mood after a deep depression can also be a red flag, as it may indicate a decision has been made.
Mood: Look for signs of severe depression, anxiety, irritability, humiliation, or rage.
The acronym IS PATH WARM is a helpful tool for remembering key warning signs: Ideation, Substance abuse, Purposelessness, Anger, Trapped, Hopelessness, Withdrawal, Anxiety, Recklessness, and Mood changes.

Underlying Risk Factors and Causes
Suicide is rarely caused by a single issue but rather a combination of factors. Key risk factors include:
Mental Health Conditions: At least 90% of people who die by suicide have a mental health disorder. Major depression increases risk twentyfold. Bipolar disorder, personality disorders, schizophrenia, anxiety, PTSD, and substance use disorders are also significant factors. Alcohol is involved in over a third of suicides.
Health Factors: Chronic pain, traumatic brain injuries, and sleep problems can contribute to suicidal thoughts.
Environmental and Historical Factors: Access to lethal means (like firearms), bullying, social isolation, a previous suicide attempt, or a family history of suicide all increase risk.
Life Circumstances: Financial or legal troubles, job loss, relationship breakups, and feeling like a burden can create overwhelming stress.
The scientific research on mental health and suicide provides deeper insight into these connections.
Specific Challenges for Youth Suicide
Youth suicide is a tragic reality. Young people face unique challenges that increase their vulnerability:
Brain Development: The adolescent brain's impulse control centers are not fully mature, which can lead to more impulsive actions on suicidal thoughts.
Social Pressures: Bullying (in-person or online) and the pressures of social media can feel devastating and heighten feelings of inadequacy and isolation.
Access to Means: Access to firearms is a critical factor, as guns are used in over half of all youth suicides in the U.S. Secure storage saves lives.
Gender Differences: While girls are more likely to attempt suicide, boys are four times more likely to die from it, often due to using more lethal methods.
For young people in Canada needing support, Kids Help Phone offers confidential help. Creating supportive environments is key to preventing youth suicide.
Finding Help and Hope: Treatment, Support, and Resources
If you or someone you know is struggling, help and hope are always available. Reaching out is an act of strength, and connection is the key to finding a way through the darkness.

How to Help Someone in Crisis
If you believe someone is in immediate danger, treat it as a mental health emergency. Your actions can be life-saving.
Ask Directly: Ask, "Are you thinking about killing yourself?" Research shows this does not plant the idea but can be a relief, showing you are willing to talk about it.
Listen Without Judgment: Let them share their feelings without arguing or offering platitudes. Validate their pain.
Keep Them Safe: If they have a plan, try to limit their access to lethal means like firearms or medications. Do not leave them alone. If an attempt seems imminent, call 911 or local emergency services immediately.
Help Them Connect: Encourage them to see a professional. Offer to help them find support or connect them with a crisis line.
Follow Up: Check in after the crisis has passed. Continued support is vital. You can also help them create a safety plan—a written guide with coping strategies and contacts for when suicidal feelings arise.
Remember what not to do: don't promise secrecy, don't try to "fix" their problems, and don't take responsibility for their feelings. Your role is to support, not to carry their burden.
Professional Treatment and Therapies
Professional treatment is key to healing. Common approaches include:
Psychotherapy: Cognitive Behavioral Therapy (CBT) helps change negative thought patterns, while Dialectical Behavior Therapy (DBT) teaches skills for managing intense emotions and distress.
Medication: Antidepressants, mood stabilizers, and some antipsychotics can be effective, especially with therapy. For young people, some antidepressants can initially increase suicidality, so careful monitoring by a doctor is essential. Newer treatments like Ketamine are also showing promise.
Hospitalization: Inpatient care provides a safe, structured environment for stabilization during a crisis.
The SAMHSA online treatment locator can help you find qualified providers.
Crisis Resources and Helplines
Immediate, confidential help is available 24/7. Save these numbers—they could save a life.
United States:
988 Suicide & Crisis Lifeline: Call or text 988. Chat online at 988lifeline.org.
Crisis Text Line: Text HOME to 741741.
Veterans Crisis Line: Dial 988 then Press 1, or text 838255.
The Trevor Project: Call 1-866-488-7386 or text START to 678-678 for LGBTQ young people.
Canada:
9-8-8: Suicide Crisis Helpline: Call or text 9-8-8. Visit 9-8-8: Suicide Crisis Helpline.
Kids Help Phone: Call 1-800-668-6868 or text CONNECT to 686868.
Hope for Wellness Help Line: Call 1-855-242-3310 for Indigenous peoples across Canada.
Prevention and Societal Impact: A Collective Responsibility
Suicide prevention is a collective responsibility that requires a public health approach. It involves building individual resilience, fostering social connections, implementing community programs, and addressing societal issues like access to mental healthcare.

Many communities are already making a difference through school programs that teach emotional regulation and workplace initiatives that prioritize mental well-being. When we talk openly about mental health and support each other, we break down the stigma that prevents people from seeking help.
The Media's Role in Prevention
The media's portrayal of suicide has a powerful impact. Sensationalized coverage that glorifies or details methods can lead to copycat acts (the Werther effect). Conversely, responsible reporting can save lives. The Papageno effect occurs when stories focus on hope, recovery, and coping strategies, encouraging vulnerable individuals to seek help.
As storytellers, A Castle on a Hill Productions is committed to creating narratives that foster understanding and inspire hope, always following suicide prevention best practices. Responsible storytelling can change perspectives and save lives.
Building a Safer Community
Creating safer communities involves practical, evidence-based strategies:
Means Restriction: Limiting access to lethal methods, such as safely storing firearms and medications, is one of the most effective prevention strategies. It creates time for a crisis to pass. Research on means restriction for suicide prevention consistently proves its effectiveness.
Policy Changes: Advocating for better access to mental healthcare, fair insurance coverage, and economic supports like stable housing addresses root causes of despair.
Education: Training people to recognize warning signs and connect those at risk with help creates a community-wide safety net. Anyone can be a "gatekeeper"—a teacher, friend, or coworker who knows how to respond in a crisis. A simple act of reaching out can be a turning point.
Frequently Asked Questions about Suicide
This is a complex topic, and it's natural to have questions. Here are clear, honest answers to some common concerns.
Why do people die by suicide?
Suicide is rarely caused by a single factor. It's typically the result of a convergence of factors, including:
Unbearable Pain: Most people who die by suicide want to end overwhelming emotional pain, not their life. They often feel trapped and see no other way out.
Mental Illness: At least 90% of people who die by suicide have one or more mental health conditions, with depression being the most common.
Psychological State: A feeling of being a burden to others is a powerful and dangerous psychological factor.
Life Stressors: Financial problems, relationship loss, chronic pain, or legal issues can act as triggers for someone already vulnerable.
Is it true that talking about suicide can make it worse?
No, this is a dangerous myth. Talking about suicide does not make it worse or plant the idea.
Asking someone directly, "Are you thinking about killing yourself?" can be a lifeline. It opens the door for them to share their pain, reduces stigma, and shows that you care enough to have a difficult conversation. Many survivors say that this direct question was the turning point that led them to get help.
What should I do if I'm having thoughts of suicide?
If you are having suicidal thoughts, know that you are not alone and these feelings are treatable and temporary. Please take these steps immediately:
Reach Out Now: Talk to a trusted person or a healthcare provider. Do not wait.
Use a Crisis Line: Call or text a crisis line. In the U.S. and Canada, you can reach help by dialing 988 or 9-8-8, respectively. These services are free, confidential, and available 24/7.
Secure Your Environment: Remove or secure any means for self-harm. Ask someone you trust for help with this. Give yourself the space to get through the crisis safely.
Recovery is possible, and treatment works. Reaching out is a sign of incredible courage.
Conclusion
As we conclude this guide, hold on to this powerful message: hope, understanding, and help are always available. We've explored the complex reality of suicide, from its definitions and statistics to the crucial warning signs. The most important takeaway is that while suicide is a major public health issue, it is preventable.
Prevention is built on connection, open conversation, and a shared commitment to support one another. Every conversation and shared resource helps dismantle the stigma around mental health and builds a more compassionate community.
At A Castle on a Hill Productions, we believe in the power of stories. With over 25 years of experience in cinematography and directing, we've seen how compelling narratives can illuminate complex topics and foster understanding. We hope this guide has shone a light on the realities of suicide and offered clear paths toward prevention and recovery.
Your role is vital. We urge you to share this guide. By spreading awareness and empowering others with this information, you become a guide of hope. Together, we can reduce stigma, improve access to care, and build a world where everyone feels supported.
For more information about our documentary work and how we use storytelling to make a difference, please visit More info about our documentary work.




Comments